Delhi Restructures Primary Care as Ayushman Bharat Centres Expand

The remaining 96 clinics were located close to newly established Ayushman Arogya Mandirs, making them redundant.
As Ayushman Arogya Mandirs continue to expand across the capital, the Delhi government has ordered the closure of 137 mohalla clinics, sharply reducing the city’s once widespread neighbourhood healthcare network.
With this move, the total number of mohalla clinics in Delhi has dropped from 167 to just 30, health officials. The decision marks a significant scaling down of a primary healthcare initiative that had expanded rapidly over the past decade.
The closure directive was communicated to Chief District Medical Officers of all districts by the mohalla clinic cell of the Directorate General of Health Services.
Officials said the decision is part of a broader restructuring of Delhi’s primary healthcare system aimed at avoiding duplication of services. Of the clinics ordered to shut, 101 were operating from porta cabins, 30 from rented premises, five from government buildings and one from a private building provided rent-free.
According to officials, 41 of the 137 clinics were already non-functional as they did not have doctors. The remaining 96 clinics were located close to newly established Ayushman Arogya Mandirs, making them redundant.
At its peak, Delhi had more than 540 mohalla clinics providing neighbourhood-level healthcare. Authorities indicated that even the remaining 30 clinics could be shut in the future as the AAM network continues to expand across the city.
Meanwhile, Chief Minister Rekha Gupta on Wednesday inaugurated 81 new Ayushman Arogya Mandirs, taking the total number of such centres in Delhi to 319. The government plans to establish around 15 AAMs in each Assembly constituency.
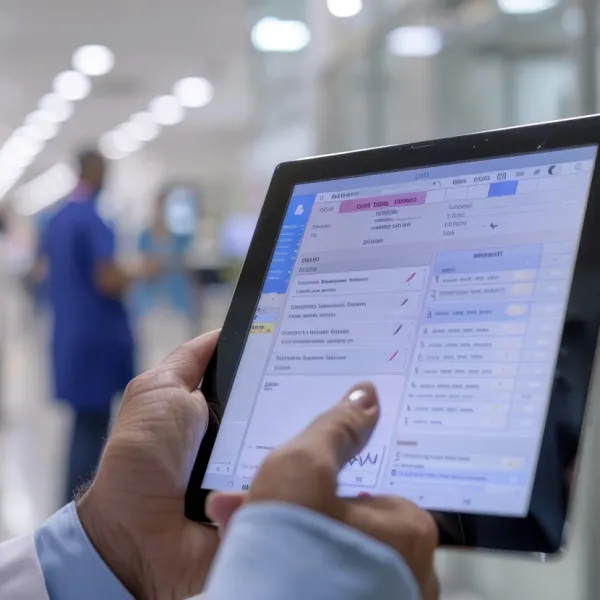
Designed as comprehensive primary healthcare centres, Ayushman Arogya Mandirs are expected to offer 12 essential service packages. These include free distribution of 161 types of medicines, 12 diagnostic tests and vaccinations for pregnant women and newborns.
The centres will also screen patients for non-communicable diseases such as cervical, breast and oral cancer. In addition, they will be equipped with video conferencing facilities, allowing patients to consult specialists at government hospitals remotely.
Stay tuned for more such updates on Digital Health News