What is Remote Patient Monitoring (RPM)? A Comprehensive Guide

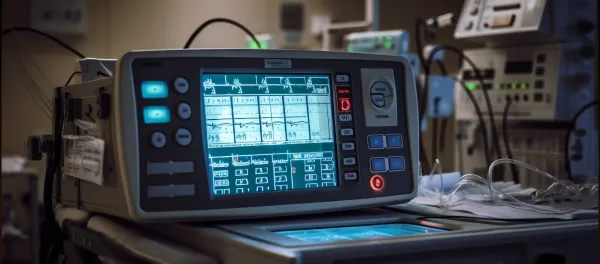
Remote Patient Monitoring (RPM) refers to the use of digital technologies and medical devices to monitor patients’ health outside of the traditional clinical setting (e.g., hospital or doctor’s office) and to transmit that health data to healthcare providers.
In effect, RPM enables the collection of patient-generated health data (PGHD) such as vital signs (blood pressure, heart rate, oxygen saturation), weight, glucose level, activity tracking, and other physiological parameters, and uses that data to support ongoing care, improve outcomes, intervene early, and shift care from reactive to proactive.
As one authoritative source puts it: “RPM is a type of telehealth in which health-care providers monitor patients outside the traditional care setting using digital medical devices.”
Why Does it Matter
- With rising chronic disease burdens, ageing populations, and resource constraints in hospitals, RPM offers a way to extend care beyond clinic walls, enhance patient engagement, and potentially reduce cost and hospital readmissions.
- The COVID-19 pandemic further accelerated interest in remote care models, supporting the need for monitoring patients at home and reducing in-person visits when appropriate.
- As healthcare systems increasingly adopt digital and connected health models, RPM is a key enabler of “care anywhere” and continuous monitoring paradigms rather than episodic visits.
Remote Patient Monitoring Devices & Use Cases
Device Type | Function | Example Use |
Blood Pressure Monitor | Tracks BP levels | Hypertension management |
Glucometer | Measures blood glucose | Diabetes care |
Pulse Oximeter | Monitors oxygen saturation | COPD, COVID-19 follow-up |
Smart Scale | Records weight trends | Heart failure care |
ECG Patch | Records heart rhythm | Cardiac monitoring |
Wearable Tracker | Measures steps, sleep, HR | Lifestyle and preventive care |
Use Cases & Clinical Applications
RPM is being used across a broad spectrum of conditions and scenarios. Some major ones include:
- Chronic disease management e.g., hypertension, diabetes, chronic obstructive pulmonary disease (COPD), heart failure.
- Post-hospital discharge monitoring / transitional care patients discharged after surgery or acute events can be monitored at home.
- Remote monitoring for high-risk or elderly patients enabling closer follow-up in home settings and reducing risk of readmission.
- Monitoring in rural or underserved settings where access to healthcare facilities may be limited.
Benefits of RPM
Implementing RPM can bring multiple advantages both for patients and healthcare systems:
- Improved access to care: Patients can be monitored without frequent clinic visits, which is particularly beneficial for mobility-limited or rural patients.
- More timely intervention and better data: Because devices can capture real-world, continuous data (not just snapshot visits), providers see more accurate trends (e.g., avoiding “white coat” effect in BP) and can intervene earlier.
- Enhanced patient engagement: Patients often feel more involved and empowered in their health management, which may lead to better self-care.
- Potential cost savings and reduced hospitalisation/readmissions: Studies suggest that RPM may reduce avoidable admissions, allow care in less intensive settings, and optimise resource use.
- Better outcomes for certain conditions: Evidence shows positive effects for certain illnesses (though not uniformly across all). For example, improved adherence, safety, and mobility have been reported.
Challenges & Limitations
While promising, RPM is not without its hurdles. Some of the major issues include:
- Data overload and workflow integration: Providers may be overwhelmed with volumes of data, or the data may not integrate cleanly with existing electronic health record (EHR) systems.
- Connectivity and technology access: Reliable internet, device usability, patient digital literacy are essential. In areas with poor connectivity or for older patients, use may be limited.
- Privacy, security and regulatory concerns: Patient data transmitted from home must be protected; devices and platforms must meet cybersecurity and compliance standards.
- Evidence base still evolving: For many patient groups and conditions, high-quality long-term studies are still limited. Some reviews indicate benefits are modest or unclear in certain contexts.
- Reimbursement and business model issues: Healthcare providers and payers must align on how RPM is reimbursed and how costs/benefits are shared.
Here’s a typical workflow for deploying RPM:
- Patient selection & consent: Identify patients who would benefit (e.g., chronic disease, high risk). Obtain informed consent for remote monitoring.
- Device setup and training: Provide home devices (BP monitor, pulse oximeter, scale, glucometer). Train the patient/caregiver on use.
- Data transmission & monitoring: Devices send data to the platform, which may flag alerts, trends or abnormal values.
- Care team review and intervention: Clinicians review data, respond to alerts (e.g., call patients, adjust treatment, schedule visit).
- Feedback & patient engagement: Patients receive feedback, adjust their behaviour (medications, lifestyle), engage with dashboards or apps.
- Continuous monitoring & adjustment: Over weeks/months, care plans may adapt based on the data trends.
- Evaluation & outcome tracking: Measure metrics such as hospital admissions, patient satisfaction, cost savings, clinical outcomes.
Key tips for successful implementation: build clinical workflows around alert triage, integrate with EHRs, ensure device usability, educate patients, address connectivity and privacy issues.
RPM in the Indian Context
While much of RPM’s development has been in high-income countries, its relevance extends strongly to India and similar markets:
In India, large rural populations, limited specialist access, and rising chronic disease burden (diabetes, hypertension, cardiovascular) make home-based monitoring an attractive solution.
However, challenges include variations in internet connectivity, device affordability, digital literacy, language, and local workflow alignment.
A successful Remote Patient Monitoring implementation in India would require: locally relevant device solutions, multilingual patient interfaces, telecom/internet access reliability, alignment with regulatory/health-insurance frameworks, and partnerships with local healthcare providers and digital health platforms.
As telehealth uptake grows in India, RPM stands to play a complementary role, especially for chronic disease follow-up, post-operative care, remote clinics, and rural outreach.
The Future of Remote Patient Monitoring
The future of Remote Patient Monitoring is AI-driven, predictive, and personalized.
Here’s what’s shaping the next generation of remote care:
- AI & Predictive Analytics: Algorithms that identify early signs of deterioration before symptoms appear.
- Wearable & IoT Integration: Multi-sensor smart patches and continuous glucose monitoring systems.
- 5G Connectivity: Ultra-fast data transmission, even in remote areas.
- Virtual Wards / Hospital-at-Home: RPM enables hospital-level monitoring at home, reducing bed occupancy.
- Value-Based Reimbursement Models: Governments and insurers are incentivizing RPM under telehealth policies.
How RPM can be Deployed
Stay tuned for more such updates on Digital Health News