Optum Launches Two AI-Powered Tools to Streamline Digital Prior Authorization

The company announced the launch of Digital Auth Complete and InterQual Auth Accelerator, two platforms aimed at automating and accelerating authorization decisions by integrating clinical data, coverage policies, and payer requirements into a more streamlined digital workflow.
Optum has introduced two new artificial intelligence-powered tools designed to reduce delays and administrative burden associated with prior authorization, a process that has long been cited as a source of friction for both providers and patients.
The company announced the launch of Digital Auth Complete and InterQual Auth Accelerator, two platforms aimed at automating and accelerating authorization decisions by integrating clinical data, coverage policies, and payer requirements into a more streamlined digital workflow.
Digital Auth Complete, supported by Humata Health, integrates directly into the electronic health record (EHR) and automates several steps in the prior authorization process. According to Optum, the platform connects with more than 250 payer systems to identify orders that require authorization and surfaces a patient’s active medical coverage for comparison with submitted clinical documentation.
Optum said the platform is expected to reduce manual touches by 45% and improve document bundling efficiency by 80%. The company also cited a projected first-pass approval rate of 96%. Allina Health, a 12-hospital system based in Minneapolis, will be the first provider to deploy Digital Auth Complete. Allina Health has previously collaborated with Optum on innovation initiatives.
“The prior authorization process has been a significant source of friction,” said John Kontor, M.D., senior vice president of clinical technology at Optum Insight. He noted that the tools are designed to bring together clinical data and evidence-based criteria to speed up decision-making.
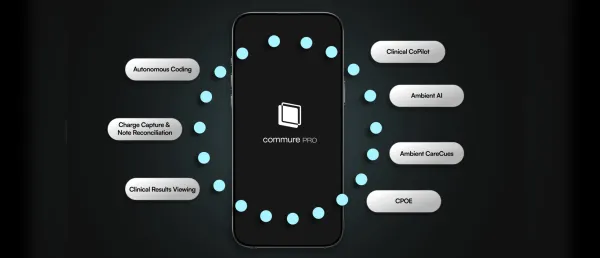
The second platform, InterQual Auth Accelerator, focuses on accelerating determinations by using trained AI models to review prior authorization submissions. The system compares requests against coverage policies and supporting documentation, then generates a recommendation for review teams, highlighting key clinical evidence within submitted materials.
Optum said the tool allows decision-makers to review cases more quickly while maintaining human oversight. The platform does not support automatic denials and enables users to customize the level of automation applied to their workflows. Based on internal testing, Optum estimates a 56% reduction in review time compared to traditional prior authorization processes.
InterQual Auth Accelerator is also positioned to help insurers meet regulatory requirements related to prior authorization and interoperability established by the Centers for Medicare & Medicaid Services. Optum confirmed it is working with a health system in New England to further evaluate the platform’s use in rethinking authorization workflows.
The newly launched tools build on Optum Real, an AI-enabled claims processing platform introduced by the company late last year, extending its use of AI across administrative healthcare processes.
Stay tuned for more such updates on Digital Health News