Healthcare's Democratization Moment: Why Complexity is Finally Forcing Transformation

Written by: Dr. Feby Abraham, Executive Vice President, Chief Strategy & Innovations Officer at Memorial Hermann Health System
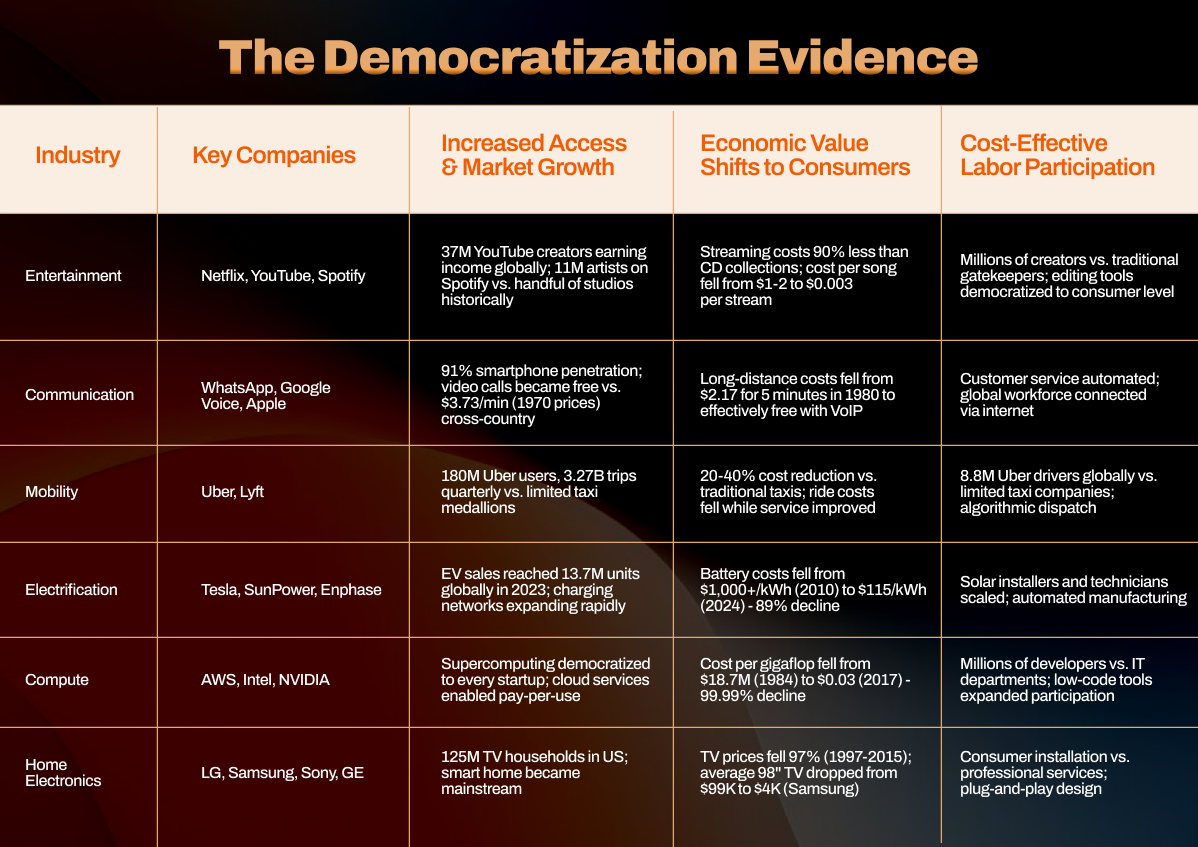
Innovation becomes democratized when three core features emerge: access expands dramatically, economic value shifts to consumers, and cost-effective labor participation increases. Entertainment, communication, mobility, electrification, computing, and consumer electronics all followed this pattern over 15-30 years. Healthcare has resisted, until now.
The uncomfortable truth: Healthcare hasn't democratized because the U.S. system provides broad access to cutting-edge innovation without rationing, but coordinates this through fragmented decision-making across employers, insurers, providers, and consumers. This multi-stakeholder architecture creates complexity and misaligned incentives that resist simplification. Multiple crises are now converging to force transformation.
The Democratization Pattern
True democratization delivers three measurable outcomes across every industry:
- Increased Access & Market Growth: Entertainment created 37 million YouTube creators earning income globally, versus a handful of studios historically. Mobility generated 180 million Uber users completing 3.27 billion quarterly trips versus medallion-constrained taxi systems.
- Economic Value Shifts to Consumers: Computing costs per gigaflop fell from $18.7 million in 1984 to $0.03 in 2017, a 99.99% decline that moved supercomputing from national labs to every startup. Battery costs fell 89% from over $1,000 per kilowatt-hour in 2010 to $115 in 2024, making EVs cost-competitive.
- Cost-Effective Labor Participation: Mobility created 8.8 million Uber drivers globally, versus limited taxi companies. Computing enabled millions of developers versus traditional IT departments through cloud platforms and low-code tools.
Healthcare's Resistance
Healthcare's scorecard reveals why democratization stalled: 20-26 day average waits for routine primary care appointments versus minutes in other industries; healthcare costs historically rise 1.7 percentage points above general inflation versus falling costs in democratized sectors; significant workforce shortage versus massive workforce expansion in computing (IT departments to millions of developers) and mobility (taxi companies to 8.8 million Uber drivers).
Healthcare faces unique structural barriers: Baumol's Cost Disease (labor-intensive, slow to automate), local and non-tradable services, licensure-capped labor supply, life-or-death stakes, regulatory complexity creating 10-15 year approval cycles, and fragmented payment architecture across multiple stakeholders with misaligned incentives. Unlike other countries that use rationing to simplify decision-making, the U.S. system attempts to coordinate access across employers, insurers, providers, and consumers, each with different objectives, timelines, and constraints.
This complexity wasn't accidental. It emerged from genuine policy goals: employer-sponsored insurance for broad coverage, multiple payers for choice, provider autonomy for quality, and consumer engagement for cost control. But the result is a coordination problem that no single actor can solve, and that resists the simplification required for democratization.
The Convergence of Economic Necessity
Multiple crises are converging to make transformation economically necessary rather than ideologically desirable.
- Unsustainable cost trajectory: Healthcare costs rise 1.7 percentage points above general inflation annually, a trajectory that projects to consume 20% of GDP by 2028. Employers and consumers can no longer absorb these increases.
- Access crisis: 20-26 day average waits for routine primary care are driving patients to emergency departments for non-urgent care, further straining the system and patient satisfaction.
- Workforce shortage: Projected deficits of 86,000 physicians and 78,000 nurses by 2036 make the current delivery model arithmetically impossible. Yet only 14-25.6% of Medicare visits use nurse practitioners or physician assistants, despite evidence showing equivalent or superior outcomes and capacity to handle 50-90% of primary care presentations.
These pressures create permission for change that policy coordination never could. When costs become unsustainable, margins compress, wait times drive patient defection, and you can't hire enough physicians, the current model's obsolescence becomes undeniable. Technology, AI-powered clinical decision support, simplified care protocols, and digital infrastructure can enable transformation. The question is whether incumbent systems will deploy these capabilities or be bypassed by those who do.
The 10-Year Inflection Point
Within a decade, traditional health systems will face an existential choice: become infrastructure orchestrators for total health management, aligning incentives across the fragmented stakeholder landscape, or become commoditized procedure factories serving platform companies that own the patient relationship and coordinate complexity on behalf of consumers.
The hospital-centric model that worked in a fee-for-service, supply-constrained environment is obsolete in a value-based, platform-enabled future. Success requires reconceiving health systems' role from providers of episodes to orchestrators of longitudinal health, coordinating across care settings, aligning stakeholder incentives, and abstracting away complexity that consumers shouldn't have to navigate.
This isn't speculation. Direct primary care bypasses insurance complexity and is growing 30% annually. Retail clinics deliver routine care safely at consumer prices. Digital health companies prove care can be delivered transparently and affordably. Major technology and retail companies are expanding delivery capabilities. The economic forces that democratized every other major industry are now present in healthcare.
The transformation will take 15-20 years, but early movers will capture disproportionate value. Unlike other industries that democratized organically, healthcare has a unique opportunity to build marketplace infrastructure deliberately, but the regulatory framework is being constructed in real-time, creating perhaps 3-5 years for platform leaders to establish dominant positions.
The question isn't whether healthcare will democratize, it's which organizations will orchestrate the stakeholder alignment versus being disrupted by those who solve coordination better. Those waiting for perfect policy alignment will discover the market doesn't wait for consensus among fragmented interests.
In Part 2, we'll explore the specific forces enabling democratization, the strategic paths organizations can pursue, and the metrics that will determine winners from those disrupted by inevitable change.
Exhibit A: The Democratization Evidence
Stay tuned for more such updates on Digital Health News