From Assistive AI to Autonomous Action: Inside Commure’s Healthcare Reset

Healthcare didn’t fail to adopt AI, it adopted it piecemeal. Over time, hospitals accumulated tools, dashboards, and copilots layered onto systems already stretched thin. What they gained in technology, they lost in cohesion. Now, with staffing shortages deepening and financial pressure mounting, health systems are no longer asking for smarter assistants. They’re asking for systems that act.
Commure CEO Tanay Tandon believes this moment marks a fundamental shift in healthcare’s AI evolution. The industry’s most urgent challenge is no longer documentation or decision support in isolation; it’s fragmentation across data, workflows, and outcomes. In response, Commure is moving beyond AI copilots toward autonomous agents that can own entire workflows, from ambient clinical documentation and coding to scheduling, eligibility checks, and revenue capture.
In this interview, Tandon explains why healthcare needs a unified AI infrastructure rather than more point solutions, how autonomous agents are already sustaining operations in community and rural hospitals, and what it takes to deploy AI that is clinically safe, context-aware, and trusted at scale. As AI moves from experimentation to execution, Commure is betting that healthcare’s future belongs to platforms that don’t just assist, but operate.
Commure sits at the intersection of ambient AI, autonomous agents, and core healthcare infrastructure. At this stage of healthcare’s AI evolution, what is the most urgent problem health systems are asking you to solve, and how has that shaped Commure’s direction over the past year?
For decades, healthcare has responded to compounding operational challenges by layering point solutions on top of already fragmented systems. What health systems are very clearly telling us now is that this approach is no longer sustainable. They don’t need more tools; they need a true platform that elegantly integrates into existing workflows.
The most urgent problem we’re being asked to solve is fragmentation: disconnected data, disconnected workflows, and AI tools that operate in isolation rather than influencing real decisions and outcomes. Over the past year, customers drove increasing focus in our roadmap on building a unified infrastructure for the revenue cycle. To bring it to life, ambient encounters now use AI to autonomously code procedures, which then in turn improves claims approvals and revenue capture. Health systems are looking to connect disparate workflows into an interconnected system that, at the end of the day, improves their financial performance.
Commure has spoken about a shift from AI copilots to AI autopilots. In practical hospital settings, particularly in community and rural hospitals, what does this shift change in day-to-day clinical and administrative workflows?
Healthcare is facing a structural labor shortage, and that pressure is most acute in community and rural hospitals. The shift from copilots to autopilots is fundamentally about where human attention is best spent.
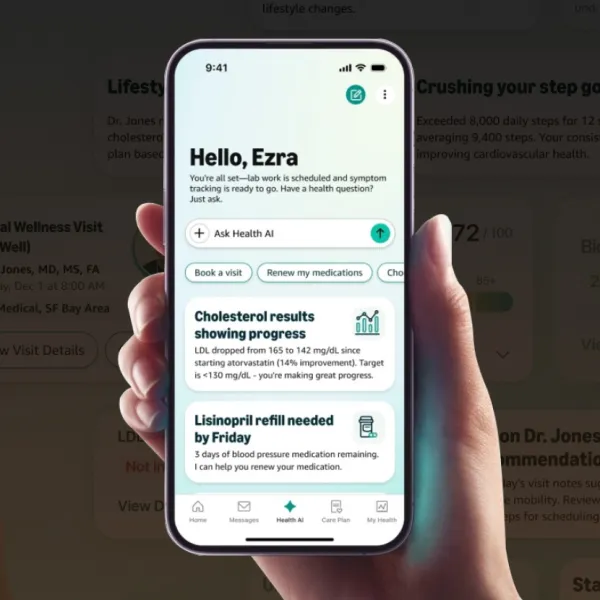
AI copilots work alongside clinicians: augmenting documentation, surfacing relevant information, and supporting decision-making in real time. For example, Ambient AI can generate clinical notes automatically and suggest CPT and ICD-10 codes, allowing clinicians to stay focused on patient care rather than administrative tasks. LLM driven longitudinal context and reasoning gives clinicians a modern-age tool kit to help them practice at the very top of their license.
AI autopilots, on the other hand, take ownership of entire workflows. These agents can operate front-office call centers, manage scheduling and patient navigation, handle eligibility checks, and initiate downstream administrative actions without requiring constant human oversight. In resource-constrained environments, that distinction matters. Autopilots don’t just save time; they allow health systems to continue operating effectively despite staffing gaps. They run 24/7/365. For example, we have seen customers capture incremental revenue simply by being able to schedule appointments that usually would have been missed.
Both approaches are essential. Copilots enhance clinical work and outcomes; autopilots sustain operational capacity.
Val Verde Regional Medical Center’s adoption of Commure Ambient AI within a MEDITECH environment is notable for a rural health system. Why was this partnership strategically important for Commure, and what does it signal about where advanced AI adoption is headed?
Val Verde is a powerful example of where healthcare AI adoption is truly headed, extending beyond large academic centers with deep IT resources to community and rural health systems that feel the burden most acutely.
This partnership is reinforcing what we’ve seen: that advanced ambient AI can be deployed successfully within a MEDITECH environment and deliver immediate value. For clinicians in resource-constrained settings, the ability to focus entirely on patients rather than screens and clicks is not a nice-to-have; it’s essential.
It also signals that AI adoption is moving beyond pilots and prestige use cases. Healthcare organizations at large are now prioritizing solutions that are practical, interoperable, and capable of working within their existing infrastructure.
You’ve described AI agents as enabling action after the clinical encounter, from scheduling procedures to managing prior authorizations. How do you ensure these agents remain clinically safe, context-aware, and trusted as they begin operating with minimal human intervention?
Our approach to how our platform and solutions are designed, governed, and implemented is rooted in our deep and sustained commitment to trust and safety. It’s a non-negotiable for us, especially as AI agents move from supporting work to taking action on behalf of health systems.
A critical part of our trust and safety foundation is clinical oversight. We have an internal clinical council composed of trained physicians and clinicians, many of whom continue to practice. This group is actively involved in shaping how all our AI agents and solutions behave in real-world settings, helping define appropriate guardrails, escalation criteria, and areas where human judgment must remain in the loop.
Equally important is how our technology is deployed. We do not believe autonomous agents can be implemented in a cookie-cutter way. Every health system has different workflows, policies, and risk tolerances. Our infrastructure is designed to support system-level customization, and our Forward Deployed Engineering teams work directly with customers to adapt agents to their specific environment. That collaboration allows us to maintain safety, context, and trust while still delivering meaningful automation.
Taken together, clinical governance, system-specific implementation, and a platform built for adaptability are what allow our agents to operate responsibly as autonomy increases.
Following Commure’s recent $200 million raise, how are you prioritizing investments across ambient documentation, revenue cycle automation, and front-office AI agents to deliver measurable ROI for health systems?
Our priority is strengthening the end-to-end platform rather than optimizing individual products in isolation. Ambient documentation, revenue cycle automation, and front-office agents are most powerful when they operate together, sharing data and reinforcing one another.
The demand by health systems for innovation has never been greater. Growth capital allows us to scale investment in product innovation, implementation, and go-to-market.
That said, we operate as disciplined, long-term stewards of our financial health. When we make incremental investments, they are tied to proven performance and allocated to accelerate innovation and improve the speed and value of what we deliver to customers.
Many hospitals struggle with fragmented AI tools layered onto legacy EHRs. Commure positions itself as unified AI infrastructure integrated across more than 60 EHRs, what has been the biggest challenge in making that promise real at scale?
There is no such thing as a “standard” healthcare deployment. Every health system has its own workflows, configurations, and constraints, regardless of the EHR.
Successful deployments depend on close, at-the-elbow collaboration with clinicians, administrators, nurses, and system leaders to drive both integration and adoption. Technology only creates impact when it is genuinely used and valued. That’s where Commure’s Forward Deployed Engineering team plays a critical role. They embed directly alongside clinicians and work with health systems to handle the necessary customization while preserving the integrity of the underlying platform.
Integration at scale is not a one-time technical achievement, it’s an ongoing operational discipline. That’s what allows us to deliver unified AI infrastructure that actually works in the real world.
Stay tuned for more such updates on Digital Health News