Digital Personal Data Protection Act (DPDP) Impact on Healthcare: A Comprehensive Study

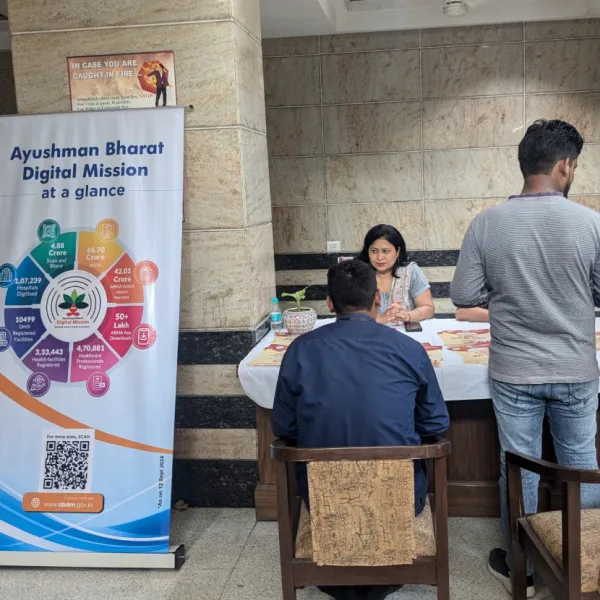
Healthcare systems worldwide are increasingly digitizing, gathering, and processing massive volumes of patient data through electronic health records, telemedicine, mobile health applications, laboratories, insurers, and health-tech platforms. Initiatives such as the Ayushman Bharat Digital Mission (ABDM) have hastened this digital transition in India. At the same time, worries over privacy, security breaches, and unauthorised data usage have intensified requests for robust legislative protections.
The Digital Personal Data Protection Act (DPDP), 2023, along with the DPDP Rules, 2025, establishes a comprehensive privacy and data protection framework in India governing how personal data is collected, processed, stored, transferred, and shared.
Given that the healthcare sector deals with extremely sensitive personal data, including medical histories, diagnoses, genetic information, and treatment profiles, the DPDP Act has the potential to drastically alter legal, operational, technological, and ethical standards throughout the Indian health sector.
Key Provisions of DPDP Act
Some key provisions of the Act include
1. Consent-Centric Data Processing -Under the DPDP regime, explicit, informed consent is mandatory for collecting and processing personal data.
2. Patient Rights and Data Principals -The Act empowers individuals (data principals) with rights such as:
- Access to their health data
- Correction and erasure requests
- Consent withdrawal
3. Data Minimization -Health data may be collected and used only for specified, explicit, and legitimate purposes such as treatment, billing, insurance verification, etc. Secondary or “secondary use” without consent is prohibited.
4. Security Measures and Breach Obligations-Healthcare organizations must adopt reasonable security safeguards, such as encryption, and in case of breaches, organizations are required to report incidents to regulatory authorities within 72 Hours
5. Accountability Governance Requirements - Entities handling health data must implement strong governance frameworks, appoint Data Protection Officers (DPOs), and conduct Data Protection Impact Assessments (DPIAs) for high-risk processing activities.
Impact of the DPDP Act On Healthcare
Given the highly sensitive nature of healthcare data, the Act has a significant impact on how healthcare organizations manage patient data. Under the DPDP Act, before collecting or processing any personal health data, healthcare practitioners must get patients' explicit, informed, and purpose-specific consent. This consent-driven framework is complemented by strengthened patient rights, enabling individuals to access their health information, correct inaccuracies, and request deletion of their data, subject to applicable medical and legal retention requirements.
Further, Hospitals are expected to adopt technical and organizational protections such as encryption, role-based access controls, secure authentication, and regular security audits to protect sensitive health data. Also, hospitals are required to create established incident response and reporting methods in order to swiftly notify the Data Protection Board and impacted persons in the case of a data breach. Under the DPDP Act, healthcare organisations remain responsible for data protection even when data is processed by third parties. Stronger contracts, vendor due diligence, and recurring compliance audits are therefore required.
The Digital Personal Data Protection (DPDP) Act further necessitates a fundamental redesign of hospital IT infrastructure, comrpising of Core digital systems, EMR/EHR platforms, Hospital Information Systems (HIS), telemedicine applications, and laboratory information systems, which must move beyond basic data storage and adopt privacy-by-design principl and they must integrate consent management, audit trails, and access controls
To comply with DPDP requirements across clinical and administrative tasks, hospitals must implement data protection governance structures, designate accountability roles, and provide staff with training.
Benefits of the DPDP Act for Healthcare
Key benefits of the DPDP Act for healthcare are -
- The DPDP Act strengthens trust between patients and hospitals by mandating patient consent and reinforcing transparency.
- The Act’s emphasis on “reasonable security safeguards” by hospitals reduces data breach risk.
- Patients acquire greater control over their personal and health information, which can foster stronger relationships and improve care outcomes.
- Supports appropriate consent for the ethical use of data for research, analytics, and innovation.
- Facilitates easier integration with interoperable health systems and national digital health initiatives.
Conclusion
The Indian healthcare industry is undergoing a radical change as a result of the Digital Personal Data Protection Act. The Act improves patient privacy and trust in digital healthcare services by mandating explicit consent, strong data governance, accountability, breach reporting, and improved patient rights. However, compliance poses financial, technical, and operational issues that need strategic planning, investment, and the implementation of privacy-by-design frameworks. As healthcare continues to digitise, the DPDP Act’s influence will likely define the next decade of data governance frameworks, potentially positioning India as a leader in privacy-conscious digital health ecosystems.
Stay tuned for more such updates on Digital Health News