Strengthening Public Health Infrastructure: India’s Digital Imperative

India’s public health infrastructure has long struggled to meet the demands of its vast and diverse population. The system faces persistent operational and logistical challenges from overburdened hospitals and uneven access to healthcare services to chronic shortages of medical personnel and inadequate primary care facilities. These shortcomings became starkly evident during recent public health crises, most notably the COVID-19 pandemic, which exposed critical gaps in service delivery, disease surveillance, and healthcare accessibility.
In this context, digital healthcare has emerged as an indispensable tool in addressing both structural inefficiencies and access barriers. The integration of technology into public health infrastructure is no longer a futuristic ambition but an immediate imperative. With innovations such as telemedicine, electronic health records, digital health IDs, and AI-driven disease monitoring systems, digital platforms are capable of expanding healthcare coverage, improving real-time data management, and enhancing clinical outcomes, especially in underserved regions. Strengthening India’s public health infrastructure through digital transformation is essential not only for crisis preparedness but for achieving equitable, accessible, and resilient healthcare for all.
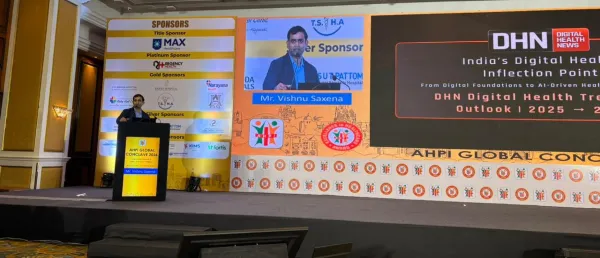
Unlock the Future of Digital Health — Free for 60 Days!
Join DHN Plus and access exclusive news, intelligence reports, and deep-dive research trusted by healthtech leaders.
Already a subscriber? Log in
Subscribe Now @ ₹499.00Stay tuned for more such updates on Digital Health News