HHS Issues Final Rule to Streamline Prior Authorizations, Boost Drug Price Transparency

The move follows a June 2025 roundtable with HHS Secretary Robert F. Kennedy, Jr., CMS Administrator Dr. Mehmet Oz, and health insurers representing coverage for nearly eight in ten Americans.
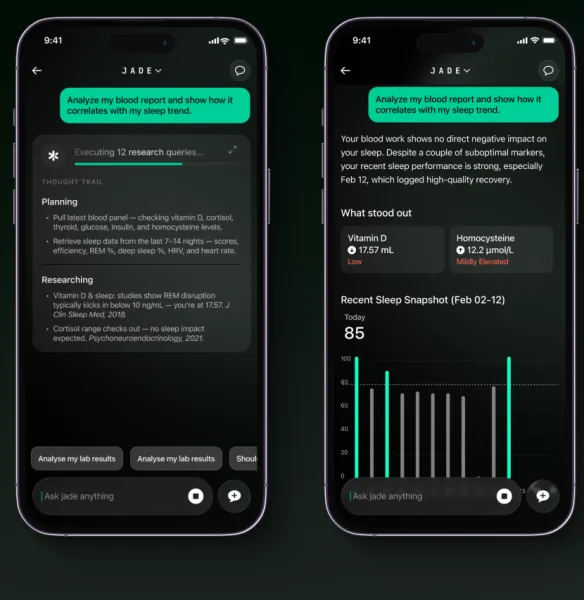
The U.S. Department of Health and Human Services (HHS) has finalized a new regulatory reform that will give doctors and patients real-time access to prescription drug information starting October 1.
For the first time, millions of Americans will be able to compare drug prices, review out-of-pocket costs, and see prior authorization requirements before treatment decisions are made.
The move follows a June 2025 roundtable with HHS Secretary Robert F. Kennedy, Jr., CMS Administrator Dr. Mehmet Oz, and health insurers representing coverage for nearly eight in ten Americans. During the meeting, insurers committed to six reforms aimed at cutting administrative red tape, speeding care decisions, and expanding transparency.
Expanding Interoperability and Cutting Burden
The rule, issued through the HHS Assistant Secretary for Technology Policy/Office of the National Coordinator for Health Information Technology (ASTP/ONC), allows providers using certified health IT systems to submit prior authorizations electronically. It also enables providers to select drugs aligned with patient insurance coverage and exchange prescription information with pharmacies and insurers.
HHS Secretary Kennedy said the rule is a step to “overhaul our nation’s broken prior authorization system.” He added that by improving patient outcomes, cutting provider burden, and ensuring transparency at the point of care, HHS is advancing its commitment to “Make America Healthy Again.”
CMS Administrator Dr. Oz noted the reforms are designed to make care “simpler, fairer, and more affordable” by providing faster decisions and reducing paperwork.
Key Policy Benefits
According to HHS, the reforms are expected to accelerate care access, enhance price transparency, and ease provider workload. Major provisions include:
Electronic Prior Authorization: Providers can submit requests electronically via certified health IT, allowing faster authorization decisions.
Drug Cost Transparency: Prescribers can compare drug prices in real time, helping patients—especially those on Medicare Part D—access cost-effective alternatives.
Reduced Administrative Burden: Workflow automation and timely decisions could save millions of clinician hours and billions in labor costs, enabling providers to focus more on patient care.
Stay tuned for more such updates on Digital Health News